KSHB 41 reporter Elyse Schoenig covers issues surrounding the cost of health care. Share your story idea with Elyse.
—
A new federal ruling from the U.S. Food and Drug Administration (FDA) now requires mammography facilities to notify patients about their breast density.
Breast density measures the amount of fibroglandular tissue in breasts.
Having dense breast tissue can make it harder to detect cancer on a mammogram.
Dr. Mary Mitchell, chief of breast radiology at Saint Luke's Health System, said having dense breast tissue also puts you at a slightly increased risk of developing breast cancer.
"On mammograms, we are obviously looking for breast cancer," Mitchell said. "The earliest signs of breast cancer, a lot of times, will start off and develop as a white area, and dense tissue is unfortunately also white."
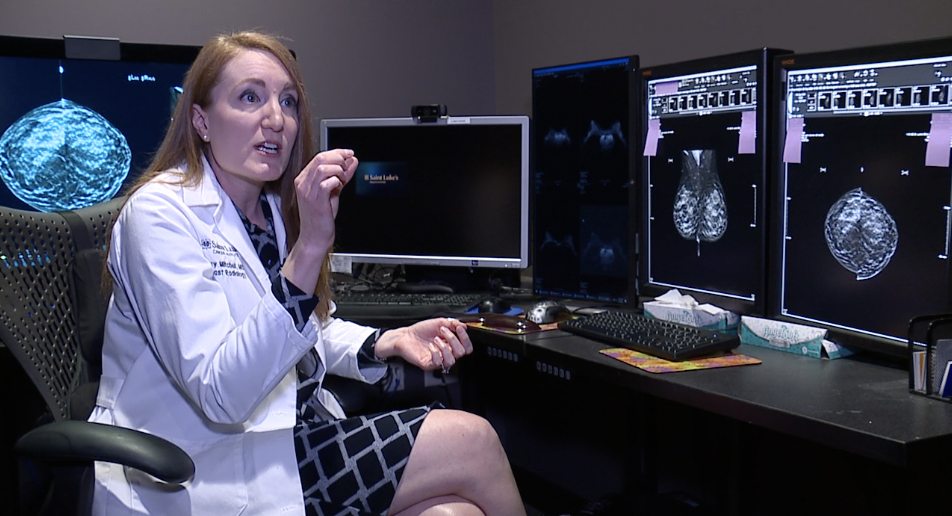
She says patients with dense breast tissue are often recommended an additional MRI or ultrasound to make sure nothing is cancerous.
"Dense breast tissue is not anything that we control," Mitchell said. "It's just sort of how we're born if we're going to have dense breast tissue or if we have more fatty breast tissue."
According to Dense Breast-info Inc., Missouri already had some breast density notification requirements in place. Kansas did not.
"Mammography is still our gold standard — [the] best screening, imaging tool that we have for detecting breast cancer," Mitchell said.
It’s why patients like Janice Thomas encourage all women to get their yearly mammogram.
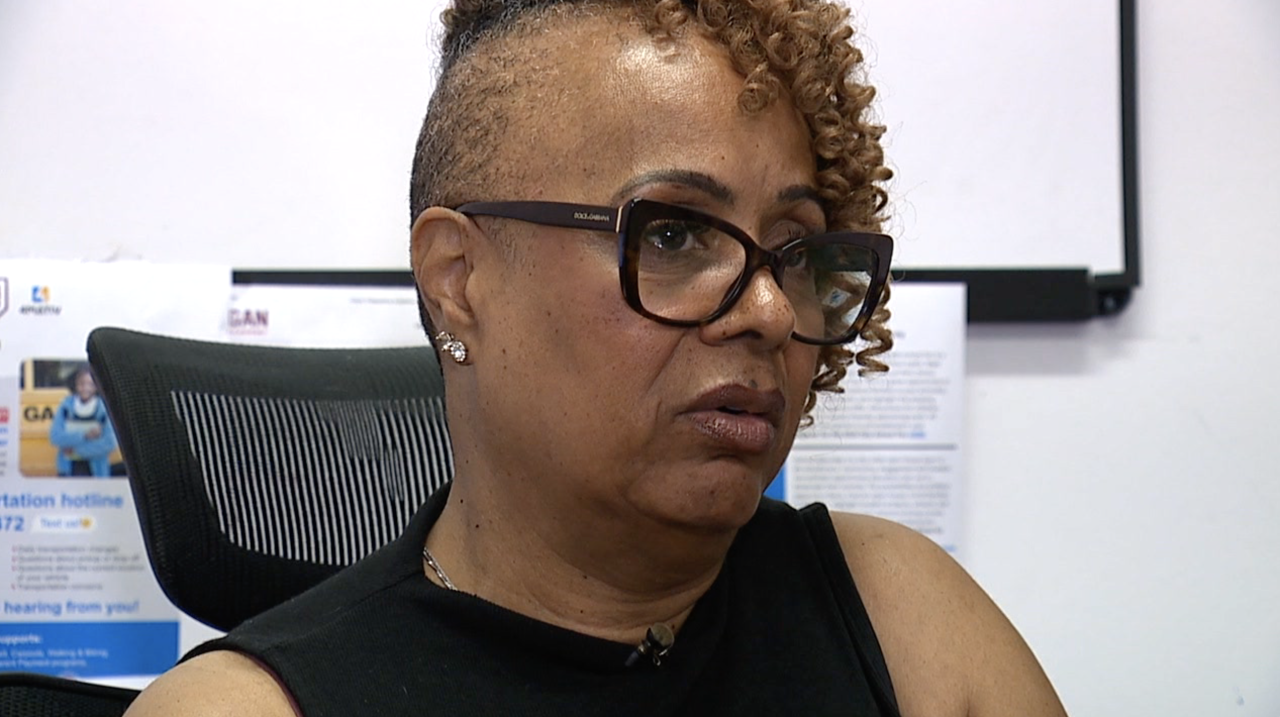
"This whole huge journey started to unfold with just one phone call," Thomas said. "Not only did I survive, but I thrived, and all because of one office visit and one test."
She's lived this way since 2015 when she found out she had breast cancer.
It was the same year she went in for her first mammogram.
"They decided they had to do the mastectomy to get the clean markers so that I would have a good chance of defeating breast cancer,” she said.
Today, Williams is grateful for life, for being cancer-free, and for mammograms.
"Since 2015, I have lived my best life," Williams said. "Doctor's appointments, taking medication, being poked and prodded to make sure everything was OK, but it was worth it."
Mitchell recommends all women get their yearly mammogram starting at age 40 if they do not have a family history of breast cancer and are not considered high-risk.
She said you should start screening, even in a primary care setting, if you do have a family history, which could mean imaging before you turn 40.
Dr. Karen Knudsen, CEO of the American Cancer Society and the American Cancer Society Cancer Action Network, shared this statement on the new federal rule:
We are particularly pleased with the inclusion of notification to patients and physicians about breast density. Dense breast tissue can make cancers more difficult to detect and is a known risk factor for breast cancer.
In addition, we applaud the inclusion of required time frames for mammography reports to be sent to healthcare providers, since delays in communication of screening results can lead to delays in diagnosis and result in worse outcomes.
Despite these advances, we maintain concern that the FDA did not include provisions to address the variability in the quality of mammography interpretation and encourage the FDA to take action on this issue immediately.
Today’s final rule will benefit all women but can help reduce the large disparity in breast cancer mortality between Black and White women. While Black and White women get screened for breast cancer at similar rates, Black women are more likely to experience lower-quality screening, contributing to the ongoing disparity.
—




